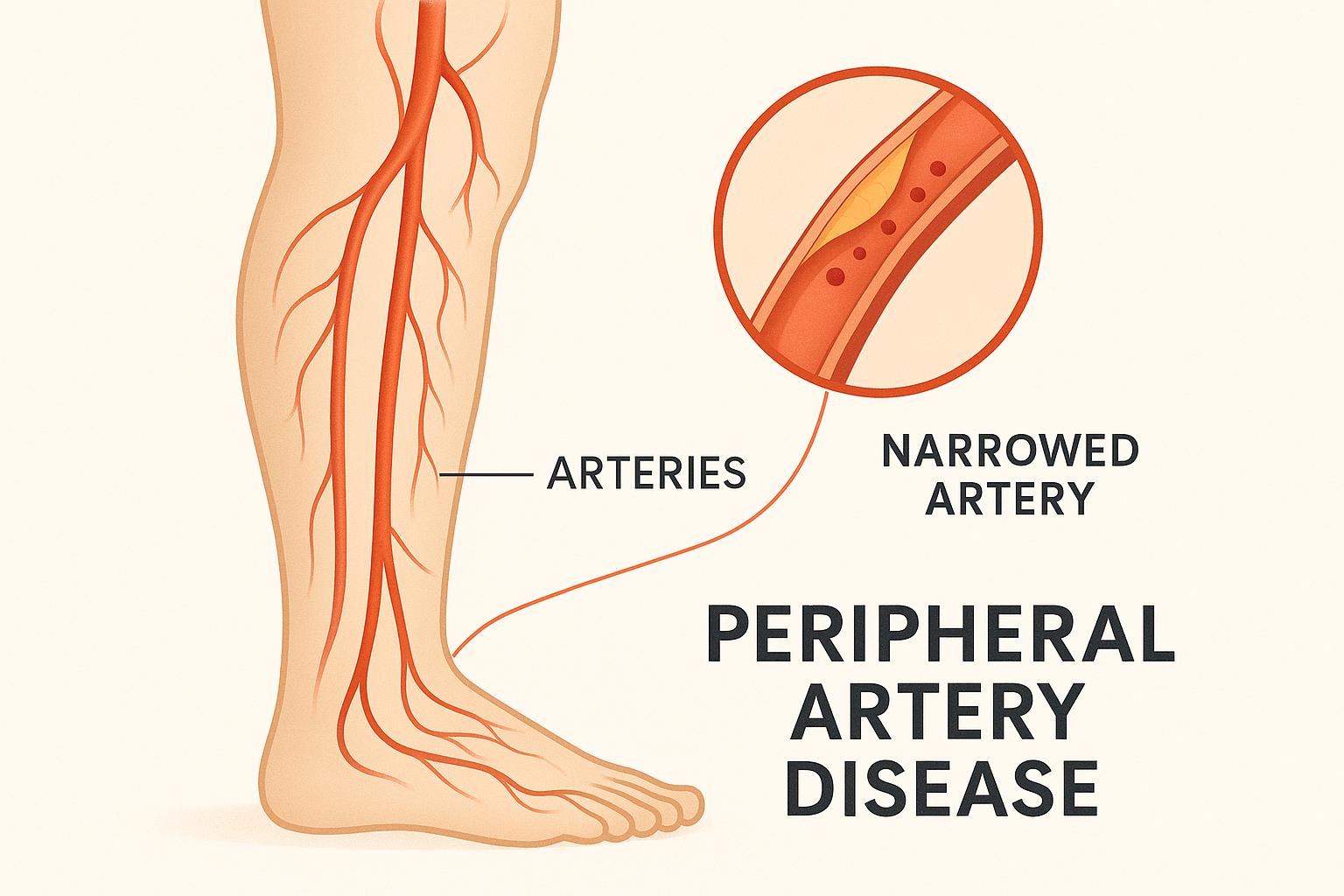
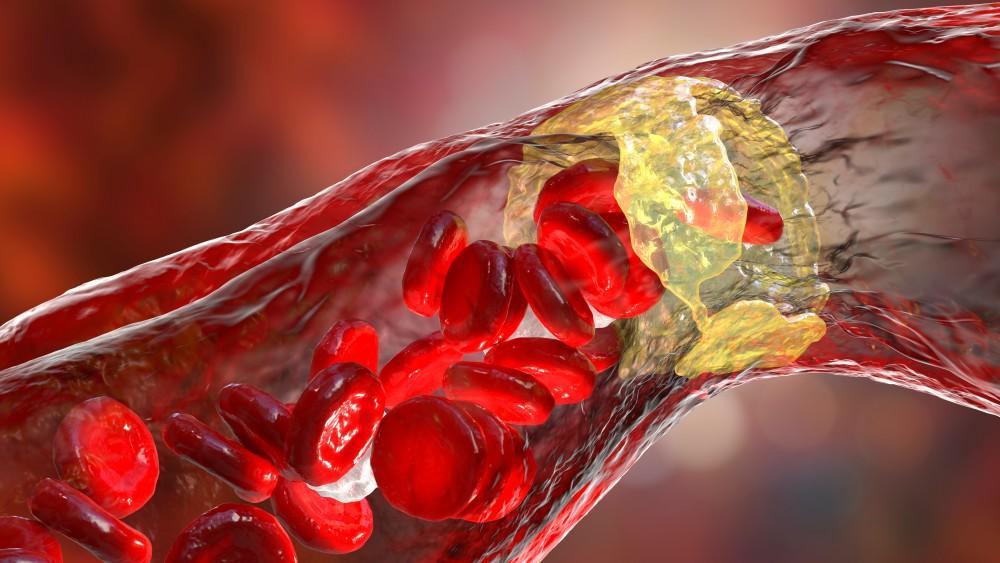
Peripheral artery disease (PAD) affects about a fifth of Americans over age 50, leaving them at risk for heart attack and stroke. PAD happens when your arteries are clogged by sticky plaques, preventing normal blood flow to your limbs and increasing your risk of dangerous blood clots.
PAD is a serious condition, and it’s normal to feel anxious about your diagnosis. There are, however, some encouraging things you should know, too.
1. PAD is treatable.
PAD is a serious medical condition, but there are highly effective ways to treat it. With proper management, you can relieve PAD symptoms and reduce your risks of serious complications, like stroke, limb disability, or amputation. The key is seeking medical treatment at the first sign of PAD or having a cardiovascular evaluation if you have PAD risk factors, even if you don’t have symptoms.
2. PAD diagnosis is simple and painless.
Speaking of symptoms and risk factors, learning to recognize both is essential for knowing when to seek treatment. PAD symptoms include:
- Limb pain that increases when exercising and improves with rest
- Temperature differences between limbs
- Slow hair growth or skin changes
- Muscle weakness or numbness in the limb
- Sores on a limb that aren’t healing
- Slower nail growth on the affected foot or hand
Because PAD is often associated with artery issues elsewhere in the body, men may also experience erectile dysfunction if they have PAD.
It’s important to know that PAD doesn’t always cause symptoms, or symptoms can be quite subtle. That’s why knowing your risk factors is also important. PAD risk factors include:
- Smoking
- High cholesterol
- Heart disease
- Diabetes
- Hypertension
- Older age (over 50)
Having a family history of PAD also increases your risk for developing it yourself.
Diagnosing PAD is a relatively simple process. In addition to reviewing your symptoms, your doctor will take your pulse in each limb, comparing the two pulses for any differences that could indicate a blockage. When PAD is suspected, noninvasive venous ultrasound provides the doctor with an “inside” view of your vessels, revealing problems that need to be addressed.
3. You don’t always need surgery.
In fact, many people with PAD relieve symptoms and reduce their risks with medication and lifestyle changes. Those changes include:
- Quitting smoking
- Increasing physical activity
- Eating a healthy diet low in fats and sugars
- Losing excess weight
Medications also typically play an important role in PAD treatment and management. Depending on your needs, you might have medicines that help prevent clots, help you manage blood pressure or cholesterol, keep your glucose level in a healthy range, or relieve limb discomfort.
4. Ongoing management can help prevent PAD in the future.
PAD isn’t a “forever” disease. With ongoing management, you can help prevent “clogging” in the future, reducing your risk of PAD and the complications it can cause. The key is to develop a management plan with your doctor and stick to it, with frequent follow-up visits to ensure your plan stays on track with your changing needs.
5. Managing PAD helps more than your limbs.
People who have clogged arteries in their limbs frequently have cardiovascular problems elsewhere, including problems with their coronary arteries or other major vessels. When you make healthy changes to manage PAD, that affects your other arteries, too. Sticking with your management plan could reduce your risks of cardiovascular disease, strokes, and other major medical issues.
If you have symptoms of PAD or risk factors for the disease, don’t put off having an evaluation. To schedule an office visit, call 972-295-7017, or book an appointment online with the team at Prime Heart and Vascular today.